Quarterly Report | Q1/2019
Supporting Whole Health
“A lot of our clients have been hurt so often - they hear what you’re saying but what’s really going to make a difference is what you do.” - Chris McClellan
Miles of flat, pine-forested land and the Okefenokee swamp cover much of the nearly 5,000 square mile, 8-county area served by Unison Behavioral Health in South Georgia. EIS coordinator Chris McClellan says, “We’re spread out. I drive up to 45 miles to get to a testing site and I might go through one little town with a single red light. The other 40 miles I see no thing but pine trees.”
Based in Waycross, Chris has been offering HIV testing, full time, for 12 years. To reach clients in numerous “small clinics and jails, two detox centers, and our new MAT program,” he stays on the road. This quarter he tested 173 people from 20 different sites.
His approach is to meet people where they are – literally traveling 100’s of miles in a day. But in a rural area where stigma around HIV and substance use tends to run high, the true meaning of meeting people where they are, says Chris, is “keeping a real open mind and realizing that if someone is in jail or a detox center it defines a decision that they made; it doesn’t define who they are.”
Don't give up. You never know when you're going to have that moment that's going to change your life or somebody else's.
“A lot of our clients have been hurt so often - they hear what you’re saying, but what’s really going to make a difference is what you do. They watch what you’re doing. Do you act like you’re embarrassed when you’re around them? Because they are really going to pick up on that. Are you taking part in the stigma or do you really feel differently?
“I think when you’re working with somebody who is in a dark place, they’re a lot more likely to get tested if they don’t feel like they’re being judged. I want people to smile when they see me. This job makes me feel like I can make people’s lives just a little bit better.”
Asked if he would like to share anything that has helped him in his work Chris replied, “Don’t give up. Just don’t ever give up. You never know when you’re going to have that moment that’s going to change your life or somebody else’s. So just keep on keeping on.”
HIV Totals, 2,797 HIV Tests, 7 New Confirmed HIV+ Diagnoses
During Q2/2019, Georgia's EIS program tested 2,797 individuals for HIV. Ot those, 99% received their results. All 7 newly diagnosed HIV-positive clients were referred to medical care; 6 were confirmed linked and one was reported to Georgia Department of Public Health for follow-up. This quarter EIS workers provided on-going support to 96 HIV+ clients, served 28 new clients previously diagnosed HIV+, and re-linked 18 who had fallen out of treatment to medical care.
HCV Totals, 2,651 HCV Screens, New HCV+ Diagnoses
During Q2/2019, Georgia's EIS program screened 2,651 individuals for HCV. Of those, 298 tested HCV Ab+ and 191 were confirmed RNA+ or chronically infected with HCV. During the same period, 150 HCV+ clients took the first step in the linkage process by completing HCV education and 43 attended their first medical appointment.
"Rarely do we have anyone not take advantage of the opportunity to learn their HIV status." - Narsheba Aasir, MARR (above right with Brandi Leichmann)
After Narsheba Aasir and Brandi Leichmann attended INSTI training in January, HIV testing at MARR in metro Atlanta more than doubled. MARR offers HIV testing to individuals with a substance use disorder in two facilities: a men’s recovery center and Right Side Up, a residential recovery center for women.
Director Marcia Smith describes Right Side Up as “a six month residential program serving 57 women. Each resident is permitted to bring up to two children aged 13 and under with them and we offer therapeutic childcare which helps lift some of the stress that women, in particular, feel coming into treatment.” Clients are referred by the Department of Family and Children Services, the State Board of Pardons and Paroles, various drug courts, and alumni.
HIV testing is a routine part of the admission process at both facilities - a component of MARR’s holistic approach to recovery. “When I sit down with clients,” says Narsheba, “we talk about a lot of things, including HIV. It’s a normal part of the conversation. I open the topic by asking what they know about HIV. That clarifies how much education they may need to understand the value of taking the test: it’s free, it’s fast, it’s confidential – and it has the potential to save lives.”
The rationale behind a whole health program, says Marcia, is that substance use “impacts every part of a client’s life; it affects them mentally, physically, and spiritually. You can’t address just one part; they all intertwine.” When clients enter treatment, most have been neglecting themselves. Many have not addressed basic medical needs. “A client may be HIV positive and off their medication. Returning to medical treatment or - for those who haven’t been tested - learning their status, is an important step toward reclaiming a healthier life.”
“I know what those families have been through,” says Jeanette. “I know first hand what addiction can do to a family; how destructive it can be – especially to children who do not understand where their mom has gone, and why don’t they see her. With every success I feel like it’s another life saved and another family spared.”
“Each patient’s success story belongs to them, but we do a lot to support their recovery. We have an excellent counseling staff that will take their calls day or night. We have a fantastic medical director who is interested in treating the person as a whole. And our nurses are all willing to go the extra mile.”
“It’s an interesting job; it’s a difficult job. Emotionally it’s very stressful. Sometimes you do all you can and a patient still relapses. But I don’t look at the people that don’t quite make it as failures. They’re not ready. When they are ready, we’ll be right here.”
“We keep moving forward every day. Today might be the day. We take every day as it comes. We do the best we can for everybody we see that day, and then we start over the next day.”
“It’s amazing to see the difference after 6 months,” says Brandi. “They hold their head higher. They haven’t worked in years and now they have a job. They’re knowledgeable about HIV and their own health needs and they have coping skills.”
“Initially, some clients are very uncomfortable with any kind of positive feedback,” says Marcia. “So for me, to witness someone who is now able hear that they have inspired others – and to see that grin on their face – is a beautiful thing.”
I don’t look at the people that don’t quite make it as failures. They’re not ready. When they are ready, we’ll be right here. - Jeanette Loudermilk, The Pittard Clinic
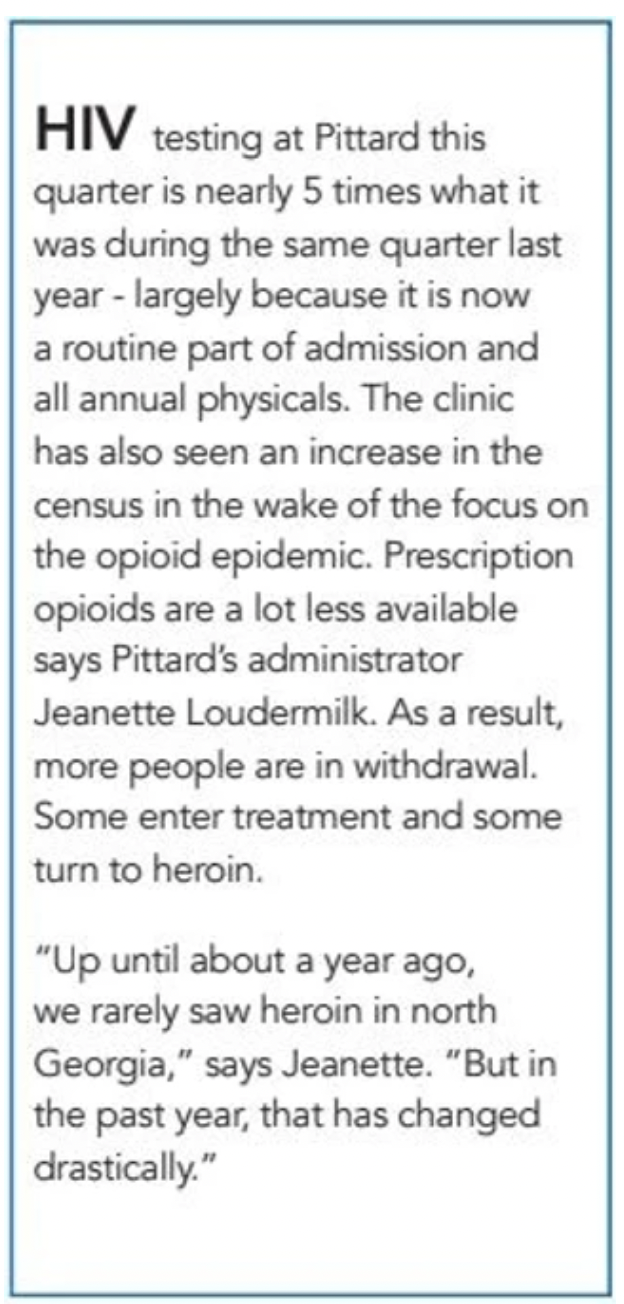
Jeanette Loudermilk has been at Pittard, a medication assisted treatment (MAT) clinic in Toccoa, Georgia for 10 years. “When I first came through those doors I thought, ‘There is no way I’m going to work in this place with this clientele.’ But I realized the clinic hours would give me time to finish school so I took the job of dosing nurse - planning to quit as soon as I got out of school.”
At that point says Jeanette she was “just like the general public.” She regarded substance use as a failure of character. “But as patients came to my window to get their medication, I listened to their stories. And it did not take me long to realize that substance use is a disease. They wanted to be well; they just didn’t know how to stop using - they needed help.”
“I could see that the people that we were serving were parents, they were somebody’s daughter, or somebody’s son. I saw patients who came in with track marks and within two or three months, those were healing and there were no fresh marks. I could see them changing, right before my eyes. They got a job, they got their children back, and they re-built relationships with family members. They were healing, and the healing was not limited to that one person - broken families were healing.”
Today Might be the Day
Meeting Clients Where They Are
As their health improves, clients grow more confident, more likely to speak up for themselves. Brandi says, “When they enter care, a lot of clients are broken. Very rarely does someone come in without a history of trauma – and for most, the trauma is compounded by shame about choices they’ve made in the past.”
Marcia adds, “We have a relationship group and a domestic violence group. You can see someone having that ‘aha moment’ when they realize, ‘Okay, that’s what I went through.’ They get to share those experiences and then explore what a healthy relationship might look like.”